An Overview of Clinical Trials
Clinical trials are research studies performed in people and test new ways to prevent, detect, diagnose, or treat diseases. They are regulated by agencies, like the Food and Drug Administration (FDA) or European Medicines Agency (EMA) and are the final obstacle in the drug development process.
The FDA defines a drug as any product that is intended for use in diagnostic, cure mitigation, treatment, or prevention of disease; and that is intended to affect the structure or any function of the body. A drug can be a chemical compound, like aspirin, that includes the types of drugs you are most familiar with, or a gene therapy.
Clinical trials progress in phases
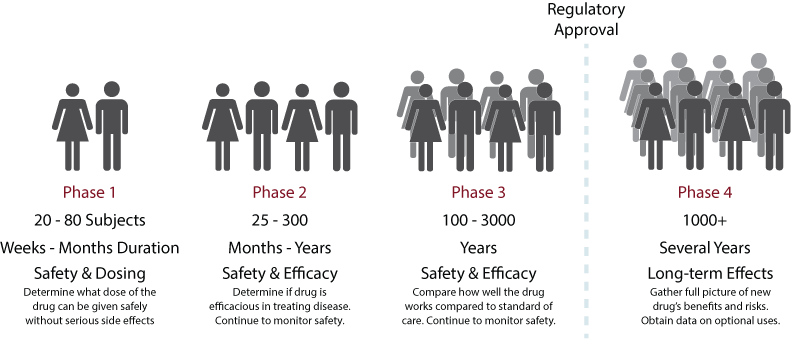
You may already be familiar with, or heard, the terms Phase 1, Phase 2, and Phase 3. Each phase is designed to address specific questions that allow the drug development and approval process to proceed further. These phases are summarized in Figure 1 and expanded on further below.
Figure 1. Phases of a Clinical Trial. Each phase of a clinical trial needs to have sufficient results that a drug is safe and has the potential to benefit patients before continuing to the subsequent phase.
Phase 1
Phase 1 clinical trials are small, meaning that the total number of patients enrolled in the trial is typically between 20 and 80; they usually last weeks to months. The goal of a Phase 1 clinical trial is not to see if the drug works but rather if it is safe. Phase 1 clinical trials are often called dose-escalation trials because these trials usually involve the application of different doses of the drug be tested; usually 3 doses, a low, middle, and high dose. These doses are determined based on data obtained in preclinical studies.
Phase 1 trials help determine what a drug’s most frequent side effects and at what doses do these side effects appear. Phase 1 trials usually progress in a step-wise manner. An initial group of subjects receive the lowest dose and are observed for any adverse reactions to the drug at that dose. If adverse reactions are absent or minor, then another group of subjects is given the next highest dose and observed (thus the dose escalates). This continues until all doses are tested or until the adverse effects become too great to increase to the next higher dose.
Because the goal of a Phase 1 study is safety, it does not necessarily need to involve people who suffer from the disease the drug is meant to treat. Phase 1 trials are often use healthy volunteers because a drug’s side effects can still be observed, but these side effects are expected to have less of an impact in a healthy person compared to people suffering from a disease. This of course depends on the type of drug being tested. For example, gene therapy drugs, which can have life-long effects, are generally not given to healthy volunteers.
Phase 2
Phase 2 clinical trials are larger, as they can include hundreds of patients, though the numbers depend on how rare a disease is. Phase 2 trials can last months to years. The goal of a Phase 2 trial is to obtain preliminary data on whether the drug works in people who have the disease the drug is meant to treat, at the dose determined from the Phase 1 trial. Additionally, safety data, including any adverse effects of the drug continue to be collected.
Phase 2 trials usually involve control groups. These are patients who receive a placebo instead of the drug. A placebo is a substance that resembles the actual drug but does not actually contain any drug, like a sugar pill. The effectiveness of the drug is determined by comparing the outcomes of the patients who received the drug compared to those who received the placebo. In some instances the inclusion of a placebo group is not possible. For example, in the case of diseases where death is imminent, denying a potentially life-saving therapy could be considered unethical. Clinical trials with certain gene therapy drugs often do not use a placebo group because a placebo version of the gene therapy could prohibit subsequent use of the active drug. In these cases, historical control data, like the data obtained in a natural history study, can be used to help determine if a drug is effective.
Often Phase 1 and Phase 2 trials are combined into a single Phase1/2 Clinical trial. In this instance the trial begins with a dose escalation approach, like a Phase 1 trial, and then when the appropriate dose is chosen, additional participants are recruited to expand that particular group and drug efficacy data is collected.
Phase 3
Phase 3 clinical trials are even larger than Phase 2 trials and can include thousands of patients; but again, this depends on how rare the disease is. Phase 3 trials usually last years. The goal of a Phase 3 trial is to gather more information about drug safety and efficacy. Because Phase 3 studies are larger, they are able to collect information on different populations of patients, for example, from larger geographical areas or different countries.
Phase 3 trials are designed to be large enough to provide regulatory agencies, such as the FDA, enough data on drug safety and efficacy to allow them to approve the drug for sale and widespread use, this called ‘market authorization’. As data is collected during these trials, changes may be made to the drug, or different subgroups of patients may be tested. It is not unusual for a drug to go through several Phase 1, Phase 2, or Phase 3 clinical trials before it obtains market authorization.
Phase 4
After a drug is approved, safety and efficacy data for that drug are still collected by regulatory agencies. This is often referred to as Phase 4. This data is collected not only from patients who may have been enrolled in the previous Phase 1 through 3 trial but new patients as well. The goal is to obtain long-term safety and efficacy data. For example, long term safety for gene therapy drugs is collected anywhere from 5 to 15 years after the first, and often only, dose. The FDA can withdraw a drug’s market authorization if long term observations uncover safety concerns.
Clinical trial participation eligibility
There is one more matter I want to discuss concerning clinical trials, and that concerns eligibility of clinical trial participants. The purpose of clinical trials is to demonstrate that a drug is safe and effective in a particular population at a particular point in time of their disease process. To obtain the cleanest and clearest data, it is important to decrease “noise” or variability in the collected data as much as possible.
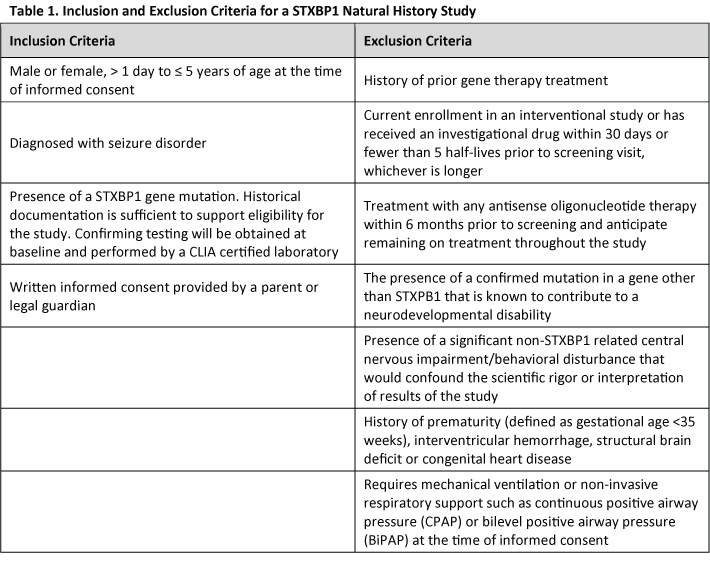
To do this, clinical trials employ inclusion and exclusion criteria when choosing participants. Every clinical trial has a set of criteria that participants must meet in order to be enrolled in the study and a set of criteria that will exclude someone from participating in the study. These criteria usually fall within certain categories such as demographics, lifestyle, gender, symptoms, co-morbidities, or other interventions.
For example, for STXBP1, a clinical trial may restrict the participants to a particular age range where it is felt the drug would have its greatest effect. To a particular area of the country, to make sure the participants can be seen in the clinic running the study. They may require participants be diagnosed with particular symptoms, like seizures. A clinical study may specifically exclude STXBP1 patients who have mutations in genes other than STXBP1 or patients who have other medical conditions such as heart disease.
Table 1 lists the inclusion and exclusion criteria for a STXBP1 natural history trial; note that this study is not a clinical drug trial, but similar criteria might be expected for a drug trial
It is important to understand that if a patient is excluded from a clinical trial, it does not mean that they will be excluded from any eventual treatment with that drug, should it be approved. Additional trials are often performed to expand the inclusion criteria to open up the drug to more subsets of patients. Additionally, if a drug is given market authorization, it could still be used by patients who did not necessarily fit the inclusion criteria of the clinical trials.
Clinical studies are complex, highly regulated endeavors, which I’ve only been able to scratch the surface of in this overview. Still, I hope you’ve gained a better understanding their important in drug development and how. Choosing to take part in a clinical trial is a very important decision, but one I hope you will consider in the future.