How Are We Going to Treat STXBP1 Disorders?
Recently a question was brought asking if supplements or drugs that mimic the action of neurotransmitters could be used to treat STXBP1. This is an excellent question, and it gives us the opportunity to discuss a larger question. How are we going to treat STXBP1 disorders?
What I mean by that question is, what are the strategies employed by scientists, doctors, and pharma companies to develop drugs for STXBP1?
Before we can answer that question though we need to understand the underlying problem that causes STXBP1 disorders. You probably already know that the disorder is caused by mutations in the syntaxin binding protein 1 gene and that this has something to do with neurotransmitters or communication between neurons.
Neurons communicate via a synapse
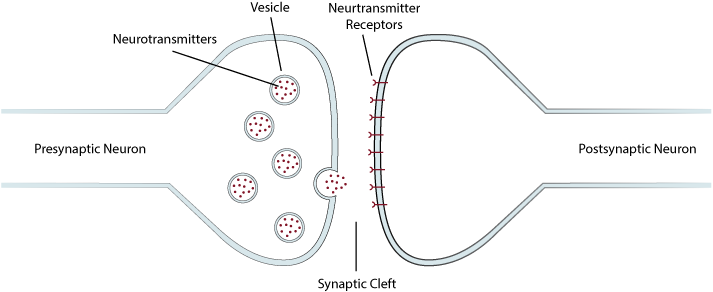
Neurons communicate with one another at a structure called the synapse (Figure 1). This is a place where the neurons come very close to one another but don’t quite touch. Neurons use neurotransmitters to communicate with one another across this synapse space. One neuron, usually referred to as the presynaptic neuron releases neurotransmitters, which in turn activate neurotransmitter receptors on the receiving neuron, usually referred to as the postsynaptic neuron. An often-used analogy is to think of neurotransmitters as pieces of mail, containing instructions, sent from one neuron to another.
Figure 1. Illustration of a Synapse. Neurons communicate with one another via synapses. A presynaptic neuron communicates with a postsynaptic neuron by releasing neurotransmitters contained in structures called vesicles into the space between the two neurons known as they synaptic cleft. The neurotransmitters then ‘attach’ to neurotransmitter receptors on the postsynaptic neuron, resulting in a response from that neuron.
There are many different types of neurotransmitters. Glutamate, GABA, dopamine, and serotonin are neurotransmitters that you may have heard of. Each type of neurotransmitter can be thought of as a specific type of mail, addressed to a specific address, or neuron, containing specific sets of instructions. For example, neurons that send out glutamate mail are generally telling other neurons to become more active, whereas neurons that send out GABA mail are generally telling other neurons to become quieter.
Neurotransmitters are stored in what are called vesicles, which can be thought of as mail bags. The function of syntaxin binding protein 1 is to help release the bag of neurotransmitter mail from a neuron into the synapse space (Figure 2). So, in a way, the STXBP1 protein is like a mail truck because it helps with delivery. One might say the problem with STXBP1 disorder isn’t that there isn’t enough mail, but rather not enough mail trucks.
Figure 2. STXBP1 is Involved in Neurotransmitter Release. In order for neurotransmitters to be released into the synaptic cleft, the vesicles containing neurotransmitters inside the presynaptic neuron have to fuse with the neuron’s cell membrane. Several proteins are involved in this process including synaptobrevin, syntaxin, and SNAP-25. Syntaxin binding protein 1 (STXBP1) is important in allowing these proteins to connect together and pull the vesicle toward the cell membrane, thus allowing it to fuse.
Mimicing neurotransmitters
So, is trying to mimic a neurotransmitter with a drug a potential approach to treat STXBP1 disorder? This may seem reasonable, but it isn’t as effective as one might initially think.
Most prescriptions drugs aimed at treating mood disorders like depression or anxiety or psychiatric problems like schizophrenia or mania work by either mimicking the action of neurotransmitters or altering their activity in some way. For example, the antidepressant drug Prozac works by increasing serotonin neurotransmission. Yet none of these types of drugs have a significant effect on STXBP1 disorder.
This is likely due to the fact that these drugs only act on one or two types of neurotransmitters whereas STXBP1 disorder affects the delivery of all types of neurotransmitters, and it is this global aspect of STXBP1 that needs to be addressed. Even if we used multiple drugs that mimicked multiple neurotransmitters, it is doubtful this would achieve the types of significant improvements in STXBP1 disorder that we would all like to see.
This is because for the brain to function properly neurotransmitter release has to be regulated. What this means is that the mail has be delivered to the correct address and at the correct time. Flooding the brain with a bunch of neurotransmitter mimics wouldn’t be regulated, it would be like dumping a bunch of letters out of an airplane and hoping they land at the correct addresses.
Having said that, it is still possible that altering the actions of one or two neurotransmitters may have positive effects on some STXBP1 symptoms, so researchers do continue to look at new neurotransmitter modifying drugs. But treating individual symptoms, while important, is not treating the whole disorder.
This is why the majority of drug development for STXBP1 disorder focuses on trying to make more, or improve the function of, the STXBP1 protein. By focusing on the STXBP1 protein, scientists are dealing with the core problem.
Approaches to treat STXBP1 disorders
One approach to do this is using gene therapy, as I discussed in a previous video. By using gene therapy, you can add a new STXBP1 gene, repair the mutant STXBP1 gene, or make the non-mutant STXBP1 gene make more normal STXBP1 protein. These gene therapy approaches are being investigated many of biopharma companies who are actively working on developing STXBP1 drugs.
Another approach is to make the STXBP1 protein that is already being made in the neurons more active. This is the idea behind the 4-phenylbutyrate trial that is currently going on. The proteins made in cells have a lifespan, meaning that they are made, they perform their function for a period of time, and then they are broken down, or recycled, like a plastic water bottle that is broken down to smaller pieces of plastic that can then be used to make a new bottle. It is thought that phenylbutyrate might increase the lifespan of STXBP1 protein by delaying its breakdown. The result is an increase in the amount of functional STXBP1 protein in the cell.
The use of 4-phenylbutyrate is an example of drug repurposing. This is taking a drug that was originally developed to treat one disease and using it to treat a completely different disease. If you watched my videos on preclinical studies in drug development and overview of clinical studies, you probably realize that it takes many years to develop a new drug and get it approved by the FDA. So if you could find a drug that is already approved by the FDA that can be used to treat STXBP1 disorder, you could save a lot of time and money.
4-phenylbutyrate was originally developed to treat a biochemical disorder in children that causes a buildup of toxic ammonia in the body. However, because of how the drug works, scientists thought it might help in protecting the STXBP1 protein.
There are thousands of drugs that have been approved by the FDA and there are companies and scientists who are trying to test many, if not all, of these drugs to see if they could help treat STXBP1 disorder. Often they are looking to see is if a drug can increase the amount of STXBP1 protein made by a cell. This is an area of research our Foundation is very interested in, and we have helped fund this type of work.
As with all science, it is always possible that with our ever-increasing understanding of the disease process that underlies STXBP1 disorder, new approaches will be discovered leading to the development of new drugs or therapies to treat the disorder. As always, I remain optimistic for the future.
Supplements
So far, I’ve discussed pharmaceutical drugs, but what about supplements? By supplement, I mean a dietary or herbal substance aimed at providing nutrients or treating a disease.
We know that diet and certain nutrients can affect brain function. For example, seizures in some STXers can be treated by using a ketogenic diet, which may work by altering the amount of a neurotransmitter called glutamate. Tryptophan, that stuff in turkey that you always hear about around Thanksgiving, has been used as a supplement to increase the amount of the neurotransmitter serotonin to treat depression. While there is some evidence that it does increase serotonin, its ability to treat depression is far less robust than pharmaceutical drugs like Prozac. About 25% of older adults take some form of supplement to improve brain health or function, but there is no solid proof that these supplements actually have any positive effect.
Pharmaceutical drugs, unlike supplements, are regulated by the FDA. This means that the FDA has determined, based on evidence from scientific testing, that the drug does have an effect on a given disease, that is, it works. The FDA also ensures that the ingredients that make up the drug are identified and safe. Supplements are not regulated by the FDA, so there is no assurance that any supplement is effective or safe.
This doesn’t mean that all supplements are unsafe or not effective, you just need to be careful if you choose to use them. For example, certain supplements are known to interact with medications, so make sure to consult your child’s doctor before you try any dietary or herbal supplements.